Lumbar Segmentation Conundrum
Submitted By: Lawrence Jankowski CBDT Affiliation: Illinois Bone and Joint Institute, LLC Morton Grove, Illinois USA
Patient History:
A 55 year old female patient, last menstrual period 2 years ago, with positive family history of maternal hip fracture (age 79). Medical history includes left wrist fracture from fall in icy parking lot 1 year ago onto a concrete barrier. No other risk factors for osteoporosis. Two different vertebral labeling schema of the spine DXA were provided by the technologist for the interpreting physician to choose from (Fig 1) as well as the right hip (Fig.2)
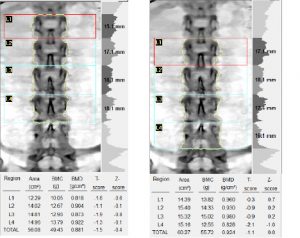
Figure 1: Two different analyses of the lumbar spine were provided by the technologist to the interpeting physician to choose from as it was unclear from the spine image as which vertebral labeling schema was correct.
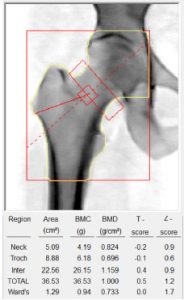
Figure 2: Right hip scan of same patient.
Questions:
- What is the etiology of the most salient visual finding in the spine scan image?
- Which, if either, of the above analyses of the spine scan would you accept?
- Answers
- This patient has six non-rib bearing vertebral segments in her lower spine. The most salient visual finding is the result of bilateral ossifications of the L5 illeo-lumbar ligaments. See the AP and oblique radiographs (Supporting images 1-2).
- The image on the right demonstrates proper vertebral labeling.
- Discussion
(Editor’s Note: The following discussion portion were graciously provided by an ISCD member radiologist, Dr. Catherine Petchprapa, who reviewed this submission for accuracy, and I cannot thank her enough for her time and assistance)
A few studies have been done regarding the use of the iliolumbar ligament to determine vertebral level numbering. Hughes et al in 2006 did a radiographic study of 500 consecutive lumbar spine MR studies and found that the iliolumbar ligament could be identified in all 432 patients with normal segmentation and was associated with L5. They concluded that the iliolumbar ligament could be reliably used to identify the L5 level. A subsequent radiographic study of 147 lumbar spine MR studies by Carrino et al in 2011 showed that the location of the iliolumbar ligament identifies the lowest lumbar type vertebra, though that level may not always be L5, with the next segment being transitional.
In addition, one should also remember that very often, hypoplastic ribs can be present at T12, and these may not be apparent on the DXA image.
Given the possibility of hypoplastic T12 ribs, the presence of the ossified iliolumbar ligaments in this case, and the appearance of a normal “sacral” level below, one could argue that the level associated with the iliolumbar ligaments is L5, and enumeration of spinal levels should follow figure 2.
Supporting Images
Supporting Image 1:

Supporting Image 1 Caption: AP Pelvis (cropped for clarity)Supporting Image 2:
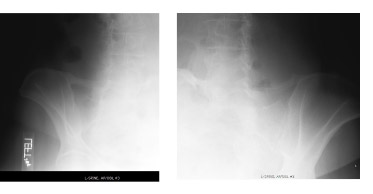
Supporting Image 2:Oblique views of pelvis (cropped for clarity)
Key Teaching Points:
- There are several segmentation variants in the lumbar spine, including four or six lumbar vertebrae, partial and complete sacralization of L5 and other variations of transitional vertebral segments which can make the identification of vertebral segment labeling subjective.
- Whenever atypical anatomic presentation is seen, additional imaging or a more careful review of the patient history, or prior radiographs or other imaging may be helpful. It is important to mention the schema you used in your analysis within the narrative of the report in case it may be needed by others should follow-up DXA examinations be required for monitoring.
References
Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR 2006
Carrino JA, Campbell PD Jr, Lin DC, Morrison WB, Schweitzer ME, Flanders AE, Eng J, Vaccaro AR. Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology 2011

