Multiple sclerotic osseous lesions in a young patient with Crohn’s disease
Title: Multiple sclerotic osseous lesions in a young patient with Crohn’s disease
Submitted by: Mounir B Errami MD PhD MBA+ and Orhan Oz MD PhD* + Parkland Hospital, 5200 Harry Hines Blvd, Dallas, TX 75235. *Corresponding author email: orhan.oz@utsouthwestern.edu, University of Texas Medical Center at Dallas, 5323 Harry Hines Blvd., Dallas, Texas 75390
Patient History: A 20-year-old male with ileocolonic Crohn’s disease diagnosed in 2014, with a reported history of steroid use for at least two months, and presently on Remicade and in remission. His course had been complicated by perianal fistulas for which he underwent fistulotomy in 2015. The patient has had several hospital admissions for Clostridium Difficile colitis (two admissions in 2018, treated with and responded to vancomycin). As part of his routine care, the patient underwent osteoporosis screening by DXA (Figure 1) following the guidelines of the American College of Gastroenterology and the American Gastroenterology Association. The patient had also complained of right knee pain. Radiographs of the knee were also obtained (Figure 2). In addition, given recurrent episodes of abdominal pain, a CT scan of the abdomen and pelvis was obtained and as axial section through the femurs was available for review (Figure 3). 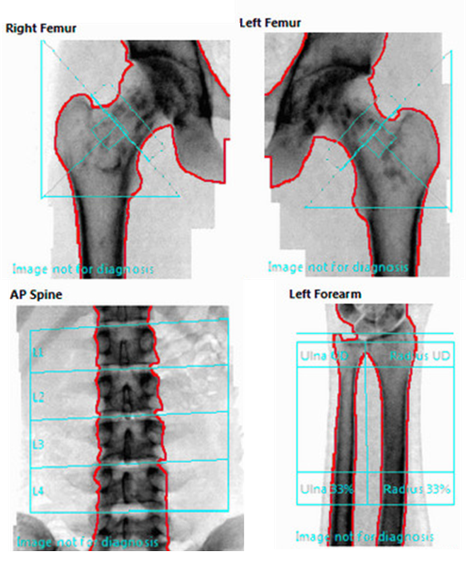
| Region | BMD (g/cm2) | T-Score | Z-Score |
| AP Spine | 1.119 | -0.9 | |
| Femur Neck Left | 1.073 | -0.3 | |
| Femur Total Left | 0.897 | -1.5 | |
| Femur Neck Right | 1.115 | 0.1 | |
| Femur Total Right | 0.939 | -1.2 | |
| Left Forearm Radius | 0.738 | -2.5 |
Figure 1. DXA scan images and BMD results for bilateral hips, and spine. Due to unusual appearance of the hip images, a forearm scan was also performed, and results are also shown.

Figure 2. AP and lateral views of the right knee.
Questions:
- Elaborate a differential diagnosis. Are any of the conditions in your differential associated to Crohn’s disease?
- Given the distribution of the lesions and their appearance, does this help refine your differential diagnosis, including any conditions not necessarily associated with Crohn’s disease?
- This patient has Crohn’s disease. Why, in your opinion, is osteoporosis suspect to the extent that it warrants evaluation by DXA?
- Does this patient have osteoporosis?
- Answers
- The differential diagnosis can essentially be divided into two categories. The first, neoplastic: sclerotic metastasis, systemic mastocytosis, and multiple healing benign or malignant lesions (after therapy). The second category, developmental: osteopoikilosis, overlap syndrome of osteopoikilosis and osteopathia striata (see knees). Other entities to consider, and that is less likely are osteoid osteoma (rarely multiple), and Erdheim-Chester histiocytosis (which would also involve the diaphysis.) None of these are particularly associated with Crohn’s disease and do not show this prototypical distribution.
- The lesions seen are polyostotic, round or oval, predominantly distributed in the epiphyses and metaphyses without architectural changes in the bone. They are periarticular, though they predominate in the long bones. This distribution is peculiar and rules out metastatic disease. As for most entities they would not necessarily be distributed in this fashion. This patient was ultimately diagnosed with osteopoikilosis, which has no relation to Crohn’s disease. Osteopoikilosis is a benign autosomal dominant sclerosing dysplasia of bone. In osteopathia striata the lesions are elongated and oval as seen in the tibial radiographs (Figures 2,3) Patients with this condition are usually asymptotic and the condition is discovered incidentally. The most common symptom is pain and it is usually treated with NSAIDs as first-line, as well as opioids when needed. The use of bisphosphonates is controversial.
- Patient’s with Crohn’s disease often use steroids for long periods of time. Osteoporosis is a known side effect of long-term steroid use. Crohn’s disease is also associated with a higher prevalence of vitamin D deficiency, as well as a link between increased inflammatory cytokine activity in active Crohn’s disease and the disruption of normal bone metabolism.
- The ISCD Official Positions (2015) state that in males under the age of 50, the diagnosis of osteoporosis cannot be made based on BMD alone. So, despite having a Z-score below -2.0, at the 33% (1/3) radius only, but spine BMD well within the range expected for age, indeterminate applicability of Z-scores in the presence of osteopoikilosis affecting the proximal femurs, no history of fragility fracture, or of long-term exposure to glucocorticosteroids for treatment of his Crohn’s disease, one could argue that this patient does not have osteoporosis. The risk of fracture in patients with osteopoikilosis at the femurs is unknown, however.
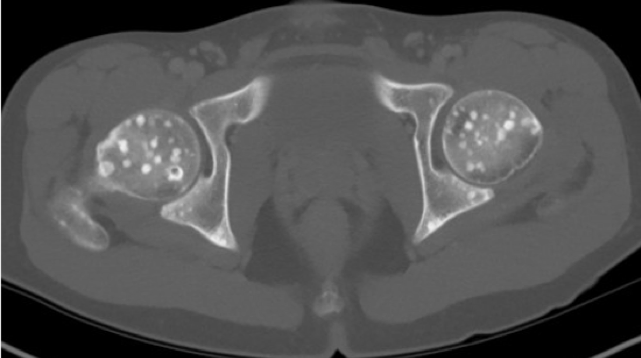
Figure 3. Axial slice through the hips at the level of the femoral heads. - Discussion
Teaching points:
- Osteopoikilosis is a rare autosomal and often asymptomatic benign sclerosing dysplasia of bone, characterized by numerous bone islands lesions are often identified incidentally.
- While the distribution of the lesions can be variable, the lesions are often in the epiphyses and metaphyses of long bones. They also typically do not affect common metastatic sites such as the skull, the ribs and the spine.
- The most common symptom is pain that tends to respond to NSAID and opioid analgesics.
- The most important alternative to consider and rule out is osteoblastic metastatic disease (e.g. breast and prostate cancer).
- It is important to review not only the BMD values and T-scores, or in this case, Z-scores, but the underlying images and their proper analyses. While “Images not for diagnoses” is an FDA required a legal disclaimer, it is not an excuse to ignore the images. Additional imaging, or a review of the medical records for recent radiographs when available, should be routine clinical practice when atypical DXA images are seen.

