Femoral Neck Size Different Between Baseline and Follow-up Scan
This is an outside facility scan. On the baseline scan the femoral neck box is 15 pixels wide. On the follow-up scan, the femoral neck box is much narrower and is not the Hologic default of 15 pixels wide
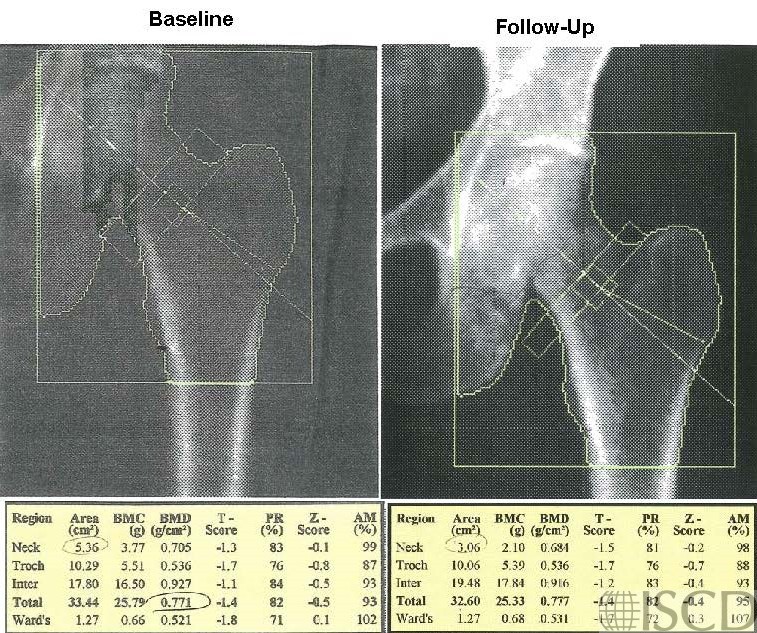
The left panel shows the baseline scan and the right panel shows the follow-up Hologic hip scan. Notice that the femoral neck box is much narrower and is not the default of 15 pixels wide on the right. This will interfere with the determination of change at the femoral neck. It is important to check and make sure that the femoral neck box is the same size on baseline and follow-up scans. This was an outside scan, so the corrected scan was not available. The patient was sent to Osteoporosis Clinic because of a concern that the femoral neck bone density was worse while on treatment. It is important to evaluate the images and technical aspects of a DXA scan. On a Hologic scan, the size of the femoral neck box and global region of interest, in pixels, is right below the image. In this case the sizes of the femoral neck box are obviously different.
Sarah L Morgan, MD, RD, CCD, The University of Alabama at Birmingham